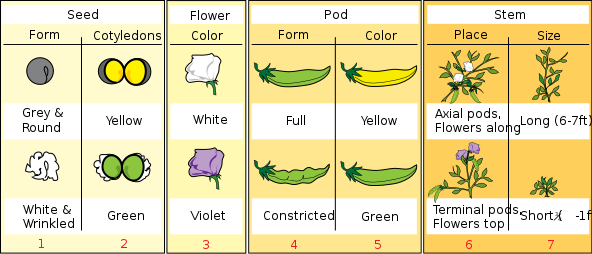
Hello, everyone! For this entry I'll be comparing a low-carb diet (or "ketogenic" diet, if you want to show off in front of your friends) with something called an "isogenic" diet.
First of all, let's define what, exactly, a ketogenic diet is (again, because repetition helps to remember things). A ketogenic diet creatively uses the term "ketogenic" because it involves the creation of ketone bodies. These ketone bodies come from the oxidation of fat in the liver; the body is able to metabolize fat because there is a shortage of glucose. The main form of glucose that humans eat come from carbohydrates, which include breads and sugars.
I have to admit something, though: the term "low-carb" is actually a bit of a lie. Carbohydrates consist of several different materials. Most people associate the term with grains and sugar only, but in actuality substances like cellulose are carbohydrates as well.
 |
| Pictured: carbohydrates. |
|
 |
| Pictured: also carbohydrates. |
The main thing about cellulose is that humans can't digest it. So, even though foods like celery are pretty much pure carbohydrate,
 |
| Green, fibrous, cellulose. |
since they're made of cellulose, you can eat as much of them as you want without getting the sugar from them.
So, calling a ketogenic diet "low-carb" is not really accurate. A more truthful definition of a ketogenic diet is a high-carb, low-glucose diet with moderate protein intake.
Isogenic diets have gained a lot of popularity in recent years with society's growing focus on all-natural, healthy lifestyle changes (gluten-free, anyone?).
Basically, the main selling point of an isogenic diet is "nutritional cleansing." People who go on this diet swear that by eating certain foods (and not eating others), they can flush out toxins in their digestive system.
 |
| Pun totally intended. |
These people say that by cleaning out toxins from the colon, people can lose weight, since, apparently, the digestive tract can hold up to 25 pounds of extra body weight.
 |
| That's as much as a really fat cat! Probably not this one, though. He's really fat. |
By replacing meals with supplements and protein shakes, the body can purge itself of toxins while still remaining fully functional and nutritionally satisfied. Unfortunately, this diet has no scientific proof of actually working, as well as no promise of long-term weight loss after initial possible weight loss.
But is there any merit to these isogenic diets? Let's look at the claim that the body can carry a large amount of excess weight in the digestive tract. This sounds an awful lot like something called visceral fat.
 |
| Aka the beer belly. |
It
is true that the body can carry extra fat in the abdominal cavity. But, as I've gone over in a previous post, visceral body fat doesn't cause insulin resistance or other metabolic problems, since the fat is contained in adipocytes and is therefore metabolically inactive. So, if you're starting an isogenic diet to fix your insulin problems because it gets rid of visceral body fat (supposedly), it's not going to help much.
The protein shake part is more interesting. A major part of ketogenic diets is their relatively high amount of protein compared to other diets, which is used in gluconeogenesis (the creation of new glucose molecules from protein) in order to keep a person's blood sugar from dropping too low. So, is that what isogenic diets do? Is it really just a ketogenic diet wearing a different hat?
 |
| "I'm so confused about which diet I'm following!" |
Well, if we look at the major supplier for isogenic diets, Isagenix, we can see that this isn't quite the case. Their chocolate protein shake has these nutrition facts:
 |
| So many numbers! |
It has 24g of protein, which is pretty good. However, in a ketogenic diet, you should really eat around 120g of protein a day, so this is only one fifth of the daily amount of protein in a ketogenic diet. And then there's the amount of carbohydrates. The total amount is 24g, but we can subtract the amount of dietary fiber, giving us 16g of sugars and other digestible carbs. This isn't so great--since I can eat a max of 50g a day, I have a little leeway when it comes to smaller numbers like this, but people on stricter ketogenic diets (like those who start in order to prevent seizures) can't have this many carbs a day.
In shorter words, the shakes are pretty low-protein in comparison to ketogenic standards, and the amount of carbs is pretty high for most people in ketogenic standards.
Plus there's the whole issue of isogenic diets possibly not working in the first place, so there's that.
Thanks for reading!